What Doctors Might Not Know Or Might Not Tell You
Since the introduction of penicillin in 1928, antibiotics have been revered as a medical marvel, effectively combating previously deadly bacterial infections and saving countless lives over the past nearly 100 years.
Today, they remain a cornerstone of modern medicine, with almost 300 million prescriptions written yearly in the United States alone… many for children and infants.
But a growing body of research casts a long shadow over antibiotics’ shining reputation.
Mounting evidence links them not only to the rise of drug-resistant “superbugs” but also to long-term health problems, weakened immunity, and even cancer. It’s becoming increasingly clear: our overdependence on “quick fix” antibiotics may be causing more harm than good.
When the Cure Becomes the Problem
Antibiotics are designed to target harmful bacteria, but they often act like a biological wrecking ball… indiscriminately wiping out both bad and good microbes in the body. This disruption of the body’s natural microbial balance, especially in the gut, can have profound consequences.
One of the most alarming concerns is the link between antibiotics and cancer. A landmark study published in the International Journal of Cancer tracked 3 million people over six years and found that those who took antibiotics just two to five times in the two years prior were 27% more likely to develop cancer. Those with six or more prescriptions faced a 37% higher risk. These findings echo other research, including a Journal of the American Medical Association study, raising red flags about the long-term cellular damage antibiotics may cause.
In addition to cancer, fatal allergic reactions—especially to common drugs like penicillin—are not uncommon. Many antibiotics also contain impurities and coloring agents that can trigger severe responses. And yet, despite the risks, physicians continue to prescribe these drugs at what some experts call “alarming rates.” Pediatricians alone account for $500 million annually in antibiotic prescriptions for ear infections, many of which are viral and not even responsive to antibiotics.
Superbugs and a Crisis of Resistance
The most well-known threat associated with antibiotic overuse is the rise of antibiotic-resistant bacteria. When antibiotics are overused, they kill off the bacteria they are designed to target, allowing resistant strains to survive, multiply, and thrive.
This creates ‘superbugs,’ which are bacteria that have become resistant to antibiotics and are, therefore, increasingly difficult to treat. These infections don’t just linger longer; they kill. And the problem is only getting worse as resistant strains outpace the development of new antibiotics.
How Antibiotics Undermine Your Health
The damage doesn’t end with resistance. Antibiotics also compromise long-term health in quieter, more insidious ways.
One major consequence is the destruction of the gut microbiome. The gut is home to trillions of beneficial bacteria that play vital roles in digestion, immunity, and even mental health. When broad-spectrum antibiotics wipe out this ecosystem, it can lead to chronic inflammation, food allergies, and malabsorption of essential nutrients. This can, in turn, cause vitamin deficiencies, immune suppression, and a cascade of health issues.
Another common outcome of antibiotic use is Candida albicans overgrowth. Normally kept in check by friendly bacteria, this yeast can proliferate when antibiotics disrupt the microbial balance, leading to persistent yeast infections and even systemic fungal problems.
Chronic fatigue syndrome, a condition characterized by persistent exhaustion and immune dysfunction, has also been linked to repeated antibiotic use. Studies show that antibiotics can weaken the immune system by disrupting enzymatic and mineral processes essential to healthy cellular function. As a result, patients often experience more frequent infections after antibiotic treatment… not fewer.
Natural Alternatives: Healing Without Harm?
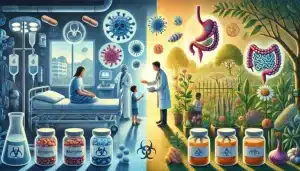
As the risks of antibiotics become more widely known, many are turning to nature for safer, effective alternatives. Long before the pharmaceutical age, healers used herbs, foods, and natural compounds to fight infection—and modern science is now validating their power.
One of the most powerful… and overlooked… tools may be high-dose vitamin C therapy. In clinical settings, high-dose vitamin C has been used as a treatment for sepsis and drug-resistant infections. It is a potent antioxidant and immune booster, helping the body fight off pathogens without harming its natural defenses.
Also, raw, unpasteurized honey has been shown to kill antibiotic-resistant bacteria like MRSA when used topically.
Thanks to its active compound, curcumin, turmeric exhibits strong antibacterial properties against pathogens like H. pylori. Oregano oil has potent antibacterial and antifungal effects, confirmed by studies in Frontiers in Microbiology.
Other natural remedies include garlic (noted for its compound allicin), which is effective against drug-resistant tuberculosis; apple cider vinegar, which has been shown to combat E. coli; cinnamon oil, which inhibits bacterial biofilm formation; and tea tree oil, which has strong antimicrobial properties.
Healthier Healthy Horizons Ahead
The modern antibiotic era may have saved millions of lives, but it’s clear that blind dependence on these drugs comes with a cost. From cancer risk and gut damage to the global rise of superbugs, antibiotics are no longer the harmless miracle pills they were once thought to be.
This isn’t about rejecting antibiotics; they remain essential in many life-threatening situations. But it’s time to reevaluate our reliance on them for every cough, cut, or childhood earache.
By supporting the body’s natural defenses and incorporating proven natural antimicrobials, we can build a more sustainable and healthier approach to healing that treats not just the symptoms but the whole person.