In the evolving landscape of neurological research, traditional diagnoses are increasingly being re-examined in light of emerging data.
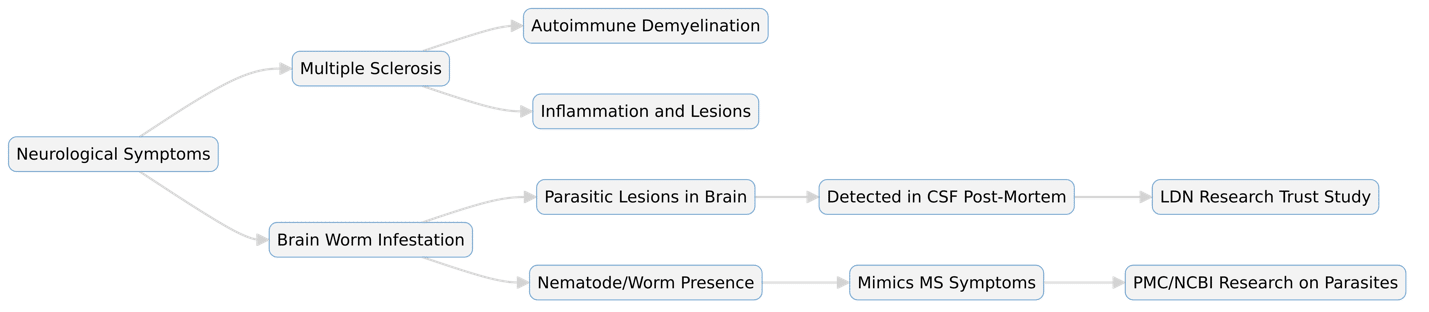
One of the more controversial claims to arise recently is the possibility that some cases of Multiple Sclerosis (MS) may actually be misdiagnosed parasitic infections—specifically, brain-invading nematodes.
This theory, proposed by Dr. Bryan Ardis and supported by selected scientific literature, challenges medical orthodoxy and prompts a reconsideration of differential diagnostics in neurology.
Understanding MS and Its Traditional Framework
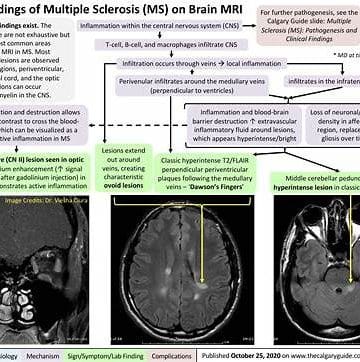
Multiple Sclerosis is characterized by immune-mediated destruction of the myelin sheath surrounding neurons in the brain and spinal cord. Its symptoms—ranging from fatigue, numbness, visual disturbances, to mobility impairments—are chronic, variable, and often difficult to conclusively trace.
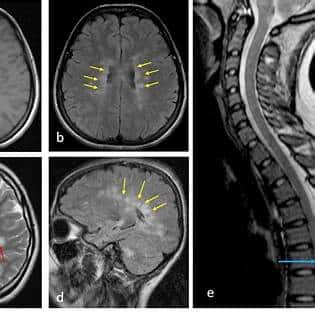
Diagnostic confirmation typically requires a combination of MRI scans, cerebrospinal fluid (CSF) analysis, and clinical symptomatology. However, none of these tools specifically test for parasitic infections, which might mimic or even cause similar inflammatory lesions and neural disruptions.
A Startling Discovery: Worms in MS-Diagnosed Brains
One foundational document in this debate is a poster study published by the LDN Research Trust. In post-mortem examinations of MS patients, nematode and filarial worms were discovered in the cerebrospinal fluid and brain tissue, raising questions about whether these parasitic infections contributed to or were mistaken for MS pathology.
These findings are not without precedent. Parasitic infections such as neurocysticercosis from Taenia solium, Toxocara canis, Onchocerca volvulus, and Strongyloides stercoralis have previously been documented to cause brain inflammation, demyelination, and severe neurological symptoms, including seizures and paralysis.
Peer-Reviewed Evidence on Parasites Mimicking Neurological Disorders
Several recent publications support the neurological effects of parasites. A 2024 study on Juglans regia (walnut leaves) demonstrated potent antiparasitic activity, offering insight into natural treatment strategies for CNS infections (source).
The National Center for Biotechnology Information (NCBI) released a comprehensive review on the neuroprotective and anti-inflammatory properties of Artemisia ludoviciana (Western wormwood) (source). Clove oil, derived from Eugenia caryophyllata, and its main component eugenol were studied for their powerful antimicrobial and nematocidal properties, relevant to potential anti-parasitic therapy (source).
Additional studies reinforce the role of inflammation and parasitic mimicry in neurodegeneration, highlighting how such infections might overlap symptomatically with autoimmune diseases (source).
Shortcomings in Standard MS Diagnosis
Typical MS treatments such as Teriflunomide (source), Dimethyl Fumarate, and Monomethyl Fumarate are designed to suppress immune activity or modulate inflammation.
While these may be effective for autoimmune disorders, they are ineffective or even harmful in cases of parasitic infection, as they dampen the body’s ability to fight intruders. This is a critical concern: immune suppression in someone with an undiagnosed parasitic infection could lead to worsening disease or death.
The absence of parasitology screenings in MS diagnostics creates a dangerous blind spot.
Toward a More Comprehensive Diagnostic Approach
Dr. Ardis argues for a paradigm shift in diagnostics. Specifically, he advocates that neurologists and general practitioners incorporate parasitic screening, especially in patients with atypical MS symptoms, unusual travel histories, or poor response to immunosuppressants.
This involves incorporating serological and PCR tests for common neurotropic parasites, using CSF antigen detection or post-biopsy analysis, and applying new imaging modalities to distinguish lesions caused by parasites from those due to autoimmunity.
It is not a call to abandon MS diagnoses but a plea for more rigorous diagnostic discrimination.
Moving Forward: Integrative and Global Perspectives
As the field of neurology increasingly intersects with immunology, infectious disease, and even global health, it’s imperative that medical professionals stay updated on overlapping presentations.
Brain worms are far more common in developing regions, yet global travel and food imports make them relevant everywhere. Additionally, integrative medicine—which includes herbal therapeutics like those derived from Artemisia, Clove, and Walnut—offers hope for adjunctive treatments.
While these are not substitutes for evidence-based pharmacology, their documented bioactivity justifies deeper exploration.
Final Thoughts
The hypothesis that some cases of MS are misdiagnosed parasitic infections is not merely speculative. It is supported by autopsy findings, backed by peer-reviewed science, and underscored by the limits of current diagnostic routines.
For patients suffering from unresponsive or atypical MS, this emerging research may offer new avenues for understanding and healing. Misdiagnosis can be catastrophic—but accurate, integrative diagnostics could change lives.
Ask your doctor if cloves, walnut leaves, and wormwood are right for you.